
A Standardized Process to Determine Appropriate and Effective Placement of Automated External Defibrillators
The new tool is an innovative, standardized method of determining the most effective placement of these necessary devices.
- By Nancy Famolare, Jane C. Romano
- Oct 01, 2016
Since the first successful open-chest defibrillation on humans in 1947 using two large silver spoons with wooden handles, the device has progressed to a portable, lightweight, life-saving tool designed to be used by non-medical individuals. Today, the automated external defibrillator (AED) constitutes the critical center link in the American Heart Association’s (AHA) Chain of Survival for victims of sudden cardiac arrest (SCA) in non-hospital settings.
If located in key locations, these devices can be the difference between life and death. Effective AED programs enable bystanders to deliver a shock to a victim within three to five minutes, increasing the chance of survival. Determining appropriate placement of AEDs requires accurate and ongoing assessment of the environment they are intended to serve.
The AHA recommends using a three-minute response time as a guideline to help determine the appropriate and most effective placement of AEDs. Using this premise, the Life Support Program (LSP) at Boston Children’s Hospital (BCH) embarked on a project to review placement of existing AEDs to support the potential impact of the devices. In collaboration with the hospital Environmental Health and Safety (EHS) department, risk assessment, heat mapping and Lean Six Sigma strategies were used to draft a tool with specific criteria and scoring to identify low-, moderate-, and high-risk areas.
Methods
In 2003, six AEDs were placed in areas throughout the approximately 2,600,000-square-foot hospital campus. Remote areas with extended emergency medical response times were targeted in this initial phase. As the hospital campus grew to what is now more than 4,200,000 square feet, so did the need for increasing the number of AEDs.
The process of determining placement continued to be focused on remote, high-risk areas that would take the hospital code team or emergency medical systems (EMS) greater than 3-5 minutes to respond. In 2013, the AED count grew to 67 machines positioned in main campus building, as well as several satellite locations.
With the expansion of the AED program, the locations of the devices were closely examined and the process of determining a standardized method of verifying the appropriate placement began. The LSP reached out to the hospital’s EHS department for help identifying risk assessment tools used for the placement of other emergency response equipment, such as fire extinguishers and eyewash stations. The strategy of risk assessment using heat mapping was explored as a method that could be applied to the program.
Heat mapping requires identifying specific factors that would contribute to an increase in risk before an assessment can be conducted. For the AED assessment, a tool was developed using the following variables:
- Is the area equipped with standard/ICU code cart/defibrillator?
- Would it take more than three minutes for emergency medical response teams to arrive?
- Is this a high-traffic area?
- Is there limited staffing/resources in this area?
- Is there limited/restricted access to this area?
- Are there identified safety/work hazards in this area?
- What is the population in this area?
A typical heat map uses colors to indicate various levels of risk. This method of warning and progressive danger is common in environmental safety circles, the most familiar being traffic lights. The tool (Figure 1) was developed to align with the hospital’s early warning scoring system, CHEWS, which also uses color to signify an increased level of concern regarding a patient’s condition. Based on this, a score of 0-8 was assigned to each location using the following scale:
- 0-2 = Green/Low-Risk Area
- 3-4 = Yellow/Moderate-Risk Area
- ≥ 5 = Red/High-Risk Area
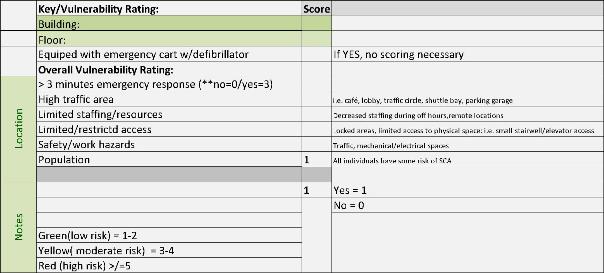 The development of the tool included plan-do-study-act (PDSA) cycles to finalize an effective scoring system. Initially, a two score system was used: yes = 1 and no = 0. After conducting assessment with this version, it was obvious the scoring method needed to be altered to reflect risk more accurately. Each variable was evaluated to determine which would most significantly influence vulnerability in an emergency medical situation. Research clearly demonstrates the critical need for early recognition and treatment of SCA in order to improve outcomes. Based on this, the decision to assign "> 3 minute code team response" a higher score if the answer was yes was made.
The development of the tool included plan-do-study-act (PDSA) cycles to finalize an effective scoring system. Initially, a two score system was used: yes = 1 and no = 0. After conducting assessment with this version, it was obvious the scoring method needed to be altered to reflect risk more accurately. Each variable was evaluated to determine which would most significantly influence vulnerability in an emergency medical situation. Research clearly demonstrates the critical need for early recognition and treatment of SCA in order to improve outcomes. Based on this, the decision to assign "> 3 minute code team response" a higher score if the answer was yes was made.
The assignment of a minimum score of 1 for population was also an adjustment made to the tool. Ideally, this variable would have a weighted score similar to a delayed response time. Several challenges were associated with developing an appropriate, simple method of assigning a score due to the fluctuating nature of the overall hospital population or, for that matter, any population. Because anyone could experience sudden cardiac arrest at any time, the decision was made to standardize this variable.
After the tool was finalized, the Lean strategy of Gemba walks was conducted using the risk assessment tool. Gemba means "the real place" and involves walking through the environment to gain a better understanding of the process and problems. This allowed for visualization of areas not typically seen or thought about by most people.
Walking into mechanical spaces, animal housing, research labs, recycling, and disposal locations proved to be an eye-opening experience. Throughout the exercise, the concept of risk was front and center. The assessment resulted in either validation of the correct placement of the existing devices or a recommendation to move an AED to a more appropriate location. Another result was the identification of 16 areas throughout the institution scoring as moderate to high risk where a AED were not readily available. Based on this assessment, hospital leadership supported the purchase and installation of the additional devices.
Even though this project was conducted in a hospital environment, it targeted mostly non-patient areas by design. Those obscure, locked, unknown areas mentioned earlier were the locations that appropriately score as moderate to high risk using the tool.
Not all of the thousands of BCH employees work at the main campus of the hospital. Several non-contiguous and satellite locations make up the more than 4,200,000 square feet the institution occupies. These locations may or may not have clinically trained people assigned and rely on local EMS for assistance when confronted with an urgent situation such as SCA. The tool was designed to be inclusive of these locations and, therefore, can be used in any environment to either validate the location of existing AEDs or identify moderate- to high-risk areas where additional devices would be beneficial.
As mentioned earlier, an essential component of having public access to AEDs is training potential rescuers. Prior to this project, an assessment of non-clinical staff's knowledge and training related to CPR and AEDs was done. A convenience sample of employees in departments such as engineering, administrative support, environmental services, research, etc. were asked the following three questions:
- Do you know what phone number to call if you need emergency medical help while at work?
- Do you know what an AED is?
- Do you know where the closest one is located?
Analysis of the results confirmed a lack of knowledge in all three areas. Strategies such as computer screen savers, "in-your-face" reminders, and hands-only training options targeting non-clinical staff were developed and implemented. A post survey conducted after three months and again a year later demonstrated a significant improvement in the awareness and understanding of these individuals related to AEDs and the institution’s emergency medical response system. These methods of strengthening the knowledge of potential rescuers remain ongoing.
The outcomes of this project are multifaceted. The newly developed tool is an innovative and standardized method of determining the appropriate and most effective placement of these necessary devices. The collaboration with the hospital's EHS department has promoted the integration of this tool and assessment into the planning of new and renovated space in the future. The most-desired and rewarding outcome of this project is the support of hospital leadership to create and maintain an environment that values the health and safety of the institution’s employees, as well as the patients and families it serves.
Conclusion
Cardiac arrest is a leading cause of death in the United States. Each year, EMS responders treat about 360,000 victims of cardiac arrest before they reach the hospital. Less than 10 percent of those victims survive. Cardiac arrest can happen to anyone at any time. It is important for companies and organizations to implement AED programs so employees are prepared to respond to a cardiac arrest emergency.
Placing AEDs in key locations and making sure employees are trained to use them can mean the difference between life and death. Implementing and maintaining an AED program requires an ongoing commitment. The devices themselves need to be monitored for mechanical functioning, such as battery life and expiration of pads. Training in the correct use of the AED needs to be current, consistent, and convenient for potential rescuers. Also important is ensuring people are aware the devices are available and how to quickly retrieve them for a medical emergency.
The value associated cannot be accurately measured in fiscal terms. It is difficult to put a price to the lifesaving potential an AED program provides.
This article originally appeared in the October 2016 issue of Occupational Health & Safety.