
A Frontline Medical Perspective on Workplace Hand Injuries
Today's safety professionals have more data at their fingertips than ever before, but simple hand lacerations continue to plague work sites, creating mountains of paperwork and productivity delays.
- By Jennifer Choi
- Jul 15, 2019
According to the CDC, hands and fingers are the most common body parts injured at work, and they represent the most frequent reason for non-fatal consultation at emergency departments (Abdelmoughit, 2017). With direct and indirect costs averaging more than $6,951 per incident, influencing both employer bottom lines and employee lives, safety professionals regularly face the challenge of reducing hand incidents on their sites (Robinson, 2016). In fact, the Bureau of Labor Statistics reported finger cuts and lacerations were the third-most-encountered causal diagnosis for time off work, resulting in an average of six lost work days (Kaya, 2011).
No one knows the frontlines of job site hand injuries like the medical professionals who treat them. Consistently, they patch workers' hands back together to keep sites running, so their insight on injury severity, trends in injury location, and hand injury recovery facts are born from real life. We asked several hand surgeons and occupational doctors a handful of industrial hand injury questions to reveal their insight into work-related hand injuries trends, causation, and recovery.
Hands: A Complex Symphony
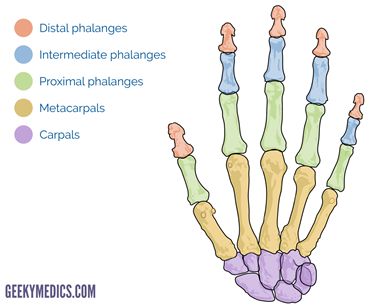
Hands are a complex symphony of delicate parts that work together. There are 27 bones, 29 joints, and at least 123 named ligaments in the human hand. About one-quarter of all our body's bones are found in our hands. The palm is uniquely protected by aponeurosis, a strong pad of tendons, which enable hands to grip things powerfully. The thumb has special functions—opposition, retroposition, palmar abduction, and radial abduction—and accounts for up to 50 percent of overall hand use (Gyer, 2018). Fun fact: The right and left hand are controlled by the opposite side of the brain.
Movements of the hand are mostly started by muscles in the forearm. There are 17,000 touch receptors and free nerve endings in the palm, sensitive to pressure, movement, and vibration.
How Hands Grip
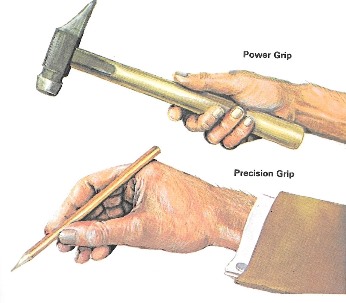
Our hands can grasp and move objects in two different ways: with a power grip or precision grip. The object’s size, shape, weight, and ease of handling determine which of these two approaches is used. The power grip is better suited for large, heavy objects, and the precision grip is used for small, delicate objects.
Occupational doctors noted repetitive wrist flexion, repetitive gripping/grasping, and repetitive use of vibratory tools lead to repetitive strain issues. To reduce the likelihood of injuries, those in manual handling roles should avoid prolonged constrained postures. Thicker handles to reduce the amount of flexion tension needed to maintain control of a tool, alternating tools and motions, and warm-up or stretching techniques can lower the risk of injury to workers who must perform manual handling tasks.
Who Gets Hand Injuries, and When Do They Happen?
Regardless whether it occurred at home or at work, almost everyone has had a hand injury at some point in their life. The injuries are a simple outcome of a body part that is both complex, delicate, and always in motion.
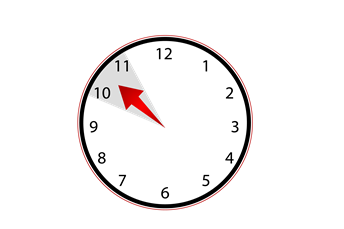
A lot of analytical software has been developed to lead organizations to believe that workplace incidents are not only trend based, but predictable. Today's safety professionals have more data at their fingertips than ever before, but simple hand lacerations continue to plague work sites, creating mountains of paperwork and productivity delays. Some of the more interesting insights gleaned from the world of big data upend common preconceived notions that the majority of hand injuries occur at the end of shifts. One study addressed temporal factors, showing a majority of hand injuries occur between 8 a.m. and noon (54.6 percent), with a peak happening from 10 to 11 a.m. (Lombardi, 2003). Private organizations that shared their data reported a similar majority of incidents occurring within the first half shifts, upending the common belief that work-weary fatigue is a leading factor.
Instead of drowning in data pools, many safety managers are investigating these injuries on the front lines with the people whose job it is to repair them. Hand surgeons report that the patients they see are split down the middle on being injured at home or at work. It doesn't tend to discriminate between men and women; the higher prevalence of male injuries is in direct proportion to the male dominance in manual labor tasks. Those who work in heavy industry tend to have more high-severity injuries, with woodwork, construction, metalwork, food handling, and textile workers most commonly affected (Rosberg 2013).
Why Do Hand Injuries Happen?
While safety managers devote their day to preventing injuries from occurring through engineering and administrative controls, those who work in the medical industry have their hypotheses on the root causes of avoidable hand injuries. Rushing, machine malfunction, and unfamiliar work tasks are common external causes that can lead to incidents. Dr. Tobias Mann, a hand surgeon at ORA Orthopedics in Iowa, agrees that distraction and fatigue are leading factors that contribute to severe hand injuries. The internal weight of stress can cause employees to lose focus on even the most basic tasks.
Acute Hand Injuries
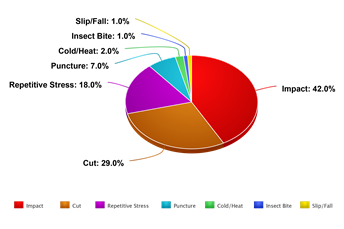
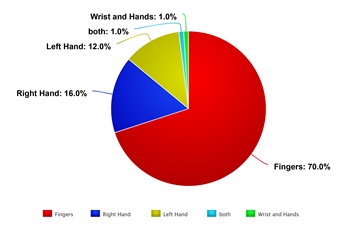
Acute injuries are the typical recordable injuries at job sites. These include caught between, pinch point, cut, puncture, bite, burn, and thermal injuries. The prevalence of injuries presented at emergency departments is to the right hand 68 percent of the time; 70 percent of the time, the fingers are affected, and the palm is nearly twice as likely to be hurt as the dorsal side of the hand (Gyer, 2018).
Most organizations purport that lacerations are the most common type of hand-related incident, but safety professionals who read incident reports in their entirety often find that punctures and avulsions get lumped into the same categories as cuts because of the presence of blood. Of the severe injuries, open fractures account for 27 percent of the injuries. Some of these include amputations, which can range from minor to life altering in scale. In many countries, the most common mechanism of injury was crush and the most common place of occurrence for hand injuries was found to be at the workplace (occupational injuries), implying a greater need for more stringent safety measures for workers (Ghiya, 2017). Mann treats crush injuries to fingertips the most often in his practice, because most minor injuries can be treated without surgery.
Overuse Injuries/Repetitive Motions
When people think of hand injuries, they normally think about acute injuries that occur violently and suddenly. Overuse injuries, such as carpal tunnel syndrome, can lead to decreased hand strength and numbness. Hand strain can equally impair hand function, and its onset is often spread over time stemming from repetitive motions.
The recent fine of Balfour Beatty Utility Solutions in the UK of £500,000 for negligently exposing employees to vibrations has caused many industries to take notice (Warburton, 2018). Attention to the citation by the HSE was not because of the fine itself, which was hefty, but because the duration of time included for the fine spanned nine years. For occupations such as physical therapy that involve repetitive hand motions, thumbs are affected 50 percent of the time, while tendon and nerve injuries are 19 percent and 13 percent, respectively (Abdelmoughit, 2017). To reduce the likelihood of onset, Mann recommends taking breaks and rotating duties and even hand positions while performing common tasks. For those seated at keyboards, adjust seating and wrist position to a zero tilt to reduce strain on the hands while typing.
The Road to Recovery
Hand injury recovery times vary, but the objective is always the same, regardless of the treatment plan. Treatment and recovery from hand injury does not rely only on technical skills of a surgeon, but also on aggressive physical therapy and the patient’s compliance (Marinković, 2015). Mann states the shortest recovery times are simple, superficial lacerations, and the longest recovery times are gunshot wounds. Doctors use a Modified Hand Injury Severity Score (MHISS) to measure functionality in a controlled way. Only 60 percent of those with major hand injuries defined by MHISS return to work (Marinković, 2015).
Reduced hand function can play a role in everyday tasks. A good outcome is defined as by regaining 75 percent of normal hand function after six months of treatment and physiotherapy. Poor outcomes lag at less than 50 percent of functionality. According to the study, after eight months, only 60 percent of patients had returned to their original occupation (Abdelmoughit, 2017).
Beyond injury severity, a few factors can influence the duration of reduced hand function. Thermal extremes can wreak havoc on "healed" injuries, disrupting the notion that things are back to normal. Despite adherence to treatment regimens, those with hand injuries often note stiffness and pain, especially when exposed to cold temperatures, for up to four years (Che, 2016).
Ignoring rehabilitation plans or cutting them short can cause a backslide in functional improvements. Leading trends in physiotherapy include purposeful activities that replicate job functions and common daily tasks to help patients improve grip and pinch strength over classic stretching. Mann sees shorter splinting times, more aggressive attention to motion and swelling, and involving fewer joints in hand surgeries as evolutions during the past decade in hand surgery. These advances in physiotherapy and improvements in hand surgery cannot be effectual if patients ghost therapy.
What's the Tipping Point Between Full Recoveries vs. Lifetime Issues?
Safety and medical professionals alike hope for a speedy return to work for those injured. The median duration of hand incident-related lost work was three days, but severe incidents can delay return to work for more than a year (Kaya, 2011). For those severely affected, a career change can cause a tumult of consequences in their personal life, finances, and professional growth opportunities. Workers' compensation benefits are both a blessing and an obstacle for injured employees on the path back to work (Shi, 2014).
Return to work (RTW) following a work-related injury is a complex process not solely determined by physical readiness. The effect of psychological issues can delay recovery (Gustafsson, 2012). Those who have a higher perceived disability tend to delay their return to work (Ramel, 2013). Injured employees may even suffer from post-traumatic stress triggered by the machinery or environment where the incident first occurred. The communication and interface style between work and the injured person can color an employee's perception of acceptance for scaled-down alternative work. Post-injury depression can creep into employees' lives if their mobility continues to be affected, spurring a trickle down of reduced performance efficiency when their normal range of opposition and abduction is impaired.
Recovery and Rehab Basics
1. Tendons
- Splints help prevent the repaired tendons being overstretched. This may last three to six weeks.
- Post tendon surgery, people can expect tendons to be back at full strength after 12 weeks, but it may take up to six months to regain the full range of movement. Expect to resume light duties after 6-8 weeks, with heavy activity delayed until after the 10-week mark.
2. Soft tissue
- Sprains and strains usually take about six weeks to heal. After 72 hours, it is important to try to start using your wrist and hand again normally to help regain full function, flexibility, and strength. Stretching exercises may be uncomfortable, but progressive resumption of activity will ensure strength and function return gradually.
3. Broken bones
- Splinting for three weeks is common. If the metacarpal bones shifted or the fracture pierced the skin, it may require surgery. Return to work is normally between 6-8 weeks.
Simple First Aid Tips for Hand Injuries
1. Clean the wound if possible and get bleeding under control.
2. Cover the wound to prevent further contamination.
3. If there is a potential fracture or dislocation, immobilize the hand to prevent further injury.
4. If there is an amputation, elevate the hand above the heart and retrieve the amputated body part.
5. Keep amputated parts clean, damp, and cool.
6. For thermal burns, cool with water and cover the injury; for chemical burns, flush with lots of water.
7. Apply ice to decrease pain and reduce swelling.
8. Remove jewelry right away, before swelling increases.
Tips for Preventing Hand Injuries Before They Happen
1. Don't use your hands to wipe away debris or shavings.
2. Power down (and lock out) equipment before dislodging jams.
3. Take your time to establish a proper grip when moving materials, especially ones that can roll.
4. Housekeeping helps—trips and falls are a common cause of hand injuries.
5. Wear PPE that is properly sized and appropriately matched to the job hazard.
References
1. Abdelmoughit Echchaoui, Leila Belaroussi, Ahmad Al Ahmad, Samir El Mazouz, Nour-eddine Gharib, & Abdellah Abbassi. (2017). Occupational hand injury patterns at Avicenna University Hospital. Hand and Microsurgery, (2), 75. https://doi-org.contentproxy.phoenix.edu/10.5455/handmicrosurg.230467
2. Che Daud, A. Z., Yau, M. K., Barnett, F., Judd, J., Jones, R. E., & Muhammad Nawawi, R. F. (2016). Integration of occupation based intervention in hand injury rehabilitation: A Randomized Controlled Trial. Journal of Hand Therapy, 29(1), 30-40. https://doi-org.contentproxy.phoenix.edu/10.1016/j.jht.2015.09.004
3. Ghiya, M. N., Murty, S., Shetty, N., & D’Cunha, R. (2017). A descriptive study of hand injuries presenting to the adult emergency department of a tertiary care center in urban India. Journal of Emergencies, Trauma & Shock, 10(1), 19–25. https://doi-org.contentproxy.phoenix.edu/10.4103/0974-2700.199519
4. Gustafsson, M., Windahl, J., & Blomberg, K. (2012). Ten years follow-up of trauma-related psychological distress in a cohort of patients with acute traumatic hand injury. International Journal of Orthopaedic and Trauma Nursing, 16(3), 128-135. https://doi-org.contentproxy.phoenix.edu/10.1016/j.ijotn.2012.03.006
5. Gyer, G., Michael, J., & Inklebarger, J. (2018). Occupational hand injuries: a current review of the prevalence and proposed prevention strategies for physical therapists and similar healthcare professionals. Journal of Integrative Medicine, 16(2), 84-89. https://doi-org.contentproxy.phoenix.edu/10.1016/j.joim.2018.02.003
6. Kaya Bicer, E., Kucuk, L., Kececi, B., Murat Ozturk, A., Cetinkaya, S., Ozdemir, O., & Coskunol, E. (2011). Evaluation of the risk factors for acute occupational hand injuries. Chirurgie de La Main, 30(5), 340-344. https://doi-org.contentproxy.phoenix.edu/10.1016/j.main.2011.04.003
7. Lombardi, D. A., Sorock, G. S., Hauser, R., Nasca, P. C., Eisen, E. A., Herrick, R. F., & Mittleman, M. A. (2003). Temporal factors and the prevalence of transient exposures at the time of an occupational traumatic hand injury. Journal of Occupational And Environmental Medicine, 45(8), 832-840. Retrieved from http://search.ebscohost.com.contentproxy.phoenix.edu/login.aspx?direct=true&AuthType=shib&db=mdc&AN=12915784&site=eds-live&scope=site
8. Marinković, M., Janjić, Z., & Nikolić, J. (2015). Estimating disability and quality of life after different degrees of hand and forearm trauma. Vojnosanitetski Pregled: Military Medical & Pharmaceutical Journal of Serbia, 72(2), 155-159. https://doi-org.contentproxy.phoenix.edu/10.2298/VSP1502155M
9. Ramel, E., Rosberg, H.-E., Dahlin, L. B., & Cederlund, R. I. (2013). Return to work after a serious hand injury. Work, 44(4), 459-469. https://doi-org.contentproxy.phoenix.edu/10.3233/WOR-2012-1373
10. Robinson, L. S., Sarkies, M., Brown, T., & O, B. L. (2016). Direct, indirect and intangible costs of acute hand and wrist injuries: A systematic review. Injury, 47(12), 2614-2626. https://doi-org.contentproxy.phoenix.edu/10.1016/j.injury.2016.09.041
11. Rosberg, H.-E., Carlsson, K. S., Cederlund, R. I., Ramel, E., & Dahlin, L. B. (2013). Costs and outcome for serious hand and arm injuries during the first year after trauma - a prospective study. BMC Public Health, 13, 501. https://doi-org.contentproxy.phoenix.edu/10.1186/1471-2458-13-501
12. Shi, Q., Sinden, K., MacDermid, J. C., Walton, D., & Grewal, R. (2014). A systematic review of prognostic factors for return to work following work-related traumatic hand injury. Journal of Hand Therapy, 27(1), 55-62. https://doi-org.contentproxy.phoenix.edu/10.1016/j.jht.2013.10.001
13. Warburton, N. (2018, June 18). "Balfour Beatty repeatedly put workers at risk of developing HAVS." Retrieved from https://www.ioshmagazine.com/article/balfour-beatty-repeatedly-put-workers-risk-developing-havs.
This article originally appeared in the July/August 2019 issue of Occupational Health & Safety.