
Industrial Exoskeletons: What You're Not Hearing
Hold on a bit longer until the capabilities of these devices match our expectations to improve human performance and reduce MSDs.
- By Blake McGowan
- Oct 01, 2018
The commercial market for technologies that augment human performance in the industrial workplace are ever-expanding. A wide range of whole-body, lower-limb, and upper-extremity devices now exist. The interest in industrial exoskeletons to improve human performance and to reduce musculoskeletal disorders (MSDs) is extremely high. Vendors and media tout the benefits of these devices, and safety professionals are eager to listen. But what do experts really know about industrial exoskeletons? And what are you not hearing?
What Are the Basics of Industrial Exoskeletons?
Let's start with the essentials.
- The definition: The Merriam-Webster dictionary defines an exoskeleton as "a wearable, external mechanical supporting structure." It is a device that augments human performance by increasing strength, endurance, and other physical capabilities of healthy or able-bodied individuals (Young and Ferris, 2017). For example, it can be used to help a person lift and carry heavy objects and support the weight of heavy tools.
- The types: These devices are classified as either active or passive. An active assistive device is powered through actuators, such as electric motors, pneumatics, levers, hydraulics, or a combination of technologies. Passive assistive devices do not include actuators; natural human movement creates the energy that powers the device through materials, springs, or dampers.
- The supported body parts: The device can be whole-body or joint-specific (for example, lower body, back, upper extremity). It can be hard or soft. Hard devices (exoskeletons) have a rigid human-device interface, which includes a solid frame and rigid structures. Conversely, soft devices (exosuits) have a lighter-weight, soft human-device interface, which includes flexible textiles.
- Standards: There is currently no established gold standard for assessing these devices for human performance augmentation (Young and Ferris, 2017). However, in 2017, ASTM International formed the ASTM Committee F48 on Exoskeletons and Exosuits to develop voluntary consensus standards for exoskeletons, including safety, quality, performance, ergonomics, and terminology for systems and components.
What Are Vendors and the Media Saying?
Until recently, the narrative around industrial exoskeletons has been controlled by vendors and the media. Most of what safety professionals know comes from these sources. Most vendors proclaim a consistent, positive message and a common set of stated benefits:
- Reduction in occupational MSDs
- Increased productivity
- Better quality of work
- Increased worker stamina
- Healthier workforce
These benefits seem very clear and concise. Unfortunately, this message is not aligned with what researchers are finding. Research shows that benefits are mixed and there are several significant physiological consequences of use.
What is Research Finding About Low-Back Industrial Exoskeletons?
To my surprise, there is very little peer-reviewed, scientific research on the benefits and consequences of industrial exoskeletons. At present, there are fewer than 100 papers published. Most evaluate the impact of devices designed to support the lower back or multiple joints during stooped working postures, dynamic lifting, static holding of a load, and general support. Unfortunately, most studies involved only one to three participants.
In general, these studies measured muscle activity (effort), muscle fatigue, and spinal loading. The positive results include the following:
- Passive devices that assist with dynamic lifting reduce muscle activity by 10 to 40 percent, reduce spinal loading by 23 to 29 percent, and reduce overall muscle fatigue (de Looze et al., 2015).
- Passive devices that assist with static trunk bending reduce muscle activity by 10 to 25 percent and spinal loading by 12 to 13 percent (de Looze et al., 2015).
However, these devices yielded some unexpected physiological consequences:
- Increased muscle activity of other joints, specifically the legs
- Increased energy expenditure (metabolic cost)
- Reduced range of motion
- Impeded motion
- Increased discomfort due to localized contact pressure
- Reduced task performance
Based on the research, the results are mixed at best.
What is Research Finding About Upper-Extremity Industrial Exoskeletons?
Over the last few years, there has been a lot of focus on smaller, single-joint devices that support the upper extremities during sustained overhead work and/or supporting heavy industrial tools in construction, petrochemical, and large-product manufacturing (airplanes, water vessels, automobiles, etc.) environments. A common goal of these devices is to reduce MSDs related to the shoulder during overhead work.
So, what do we know about the passive, upper-extremity exoskeletons used for sustained, overhead work and/or heavy tool use? Data shows the results are mixed, as well.
Impact on reducing occupational MSDs when wearing an upper-extremity device
There is no peer-reviewed scientific research that has investigated or measured the impact that upper-extremity devices have on reducing MSDs. Thus, the potential impact on reducing upper-extremity MSDs is unknown (Rashedi et al., 2014).
However, recent research provides some insights on spinal loading (force experienced by the lower back) while wearing an upper-extremity device. Spinal load is one of the primary risk factors for lower-back pain (Marras, 2012, and NCR, 2001). The peer-reviewed scientific research findings are mixed.
- Some show that the compressive forces decrease by 19 percent and that shear forces decrease by 30 percent (Kim et al., Part II, 2018).
- Others found that the device increased compressive forces by 38 to 57 percent and increased shear forces by 30 percent (Weston et al., 2018), implying that these devices could negatively affect the lumbar spine and possibly lead to injury.
Impact on productivity and quality of work
There is little peer-reviewed scientific research on the impact of upper-extremity devices on task performance, including productivity and quality of work. Again, the results are mixed.
- Some show reductions in task time by 19 percent (Kim et al., Part I, 2018).
- Others have seen an increase in task time by 30 percent (Theural et al., 2018).
Additionally, quality errors seem to significantly increase during use (Kim et al., Part I, 2018).
Impact on worker stamina and health
There is more peer-reviewed scientific research on the impact on worker stamina, including measures of muscle activity (a physiological measurement of effort), muscle fatigue, and perceived discomfort.
The impact on muscle activity includes the following:
- Reduced muscle activity in the shoulder by 36 to 73 percent (Kim et al., Part I, 2018; Rashedi et al., 2014; Theural et al., 2018) and in the (back of) arm by 40 percent (Rashedi et al., 2014)
- Increased muscle activity in the (back of) arm by 95 to 116 percent (Theural et al., 2018)
- Increased low-back muscle activity and demand by 31 to 120 percent (Rashedi et al., 2014; Theural et al., 2018; Weston et al., 2018)
- Increased abdominal muscle activity by 42 to 66 percent (Weston et al., 2018)
- Increased (front) lower leg muscle activity (Theural et al., 2018)
It appears that the use of upper-extremity devices is not reducing the load on the human, just shifting the load from the shoulders to the lower back and legs. Ideally, a properly-designed device should reduce the load on the joint of interest (shoulder) without direct cost to another region of the body (low back or legs).
Localized muscle fatigue decreases with the use of the upper-extremity device, especially for the upper arms and shoulders, but there's no impact on the lower back (Rashedi et al., 2014).
The perceived discomfort rating is a way to measure the physical activity intensity level (how hard you feel your body is working). To be deemed useful, a well-designed upper-extremity exoskeleton should reduce perceived discomfort for all body areas. Currently, the results are mixed. Some studies show no impact or benefit on perceived physical discomfort for the neck, shoulders, upper arm, upper back, lower back, or legs (Kim et al., Part I, 2018). Other studies found decreases in perceived physical discomfort in the forearm (Kim et al., Part I, 2018), upper arm by 54 to 57 percent, and shoulders by 34 to 45 percent (Rashedi et al., 2014). There have also been reported increases in perceived physical discomfort by 24 to 48 percent (Rashedi et al., 2014).
Impact on preference for use
When participants were asked for their preference to use the device, some reported they would gladly use it (Rashedi et al., 2014), while most said they did not perceive a real improvement (Theural et al., 2018) and others preferred not to use them (Weston et al. 2018). Participants perceive the devices as uncomfortable and providing a poor/loose/unresponsive fit (Rashedi et al., 2014; Weston et al., 2018).
Other concerns
Beyond the typical performance metrics, there are other concerns related to using an upper-extremity device:
- Energy expenditure and cardiovascular effort increase by 14 percent (Theural et al., 2018, and Young and Ferris, 2017).
- Kinematic strain (movement constraints) increases (Theural et al., 2018) and results in fewer torso movements (Rashedi et al., 2014) and reduced shoulder range of motion by 10 percent (Kim et al., Part II, 2018).
- Posture strain and instability increase (Kim et al., Part II, 2018, and Theural et al., 2018).
- They don't always move in the natural plane of motion.
- They can be costly, ranging from $4,000 to $7,000 per device.
In all, there are unknown safety concerns and a lack of understanding of how the device might increase muscle deconditioning and muscle atrophy.
Are They Ready for Prime Time?
In simple terms, the potential for industrial exoskeletons to improve human performance and possibly reduce MSDs is tremendous. Unfortunately, we know little about the physiological benefits and the unexpected consequences. Since there seems to be an equal number of both, the devices are not quite ready for prime time. But we are likely a decade away from a fully functional device that can provide the benefits with few consequences.
Research by Gartner, a leading research and advisory company, indicates in all aspects of business related to emerging technologies, human augmentation devices (industrial exoskeletons) for healthy or able-bodied individuals are more than 10 years away.
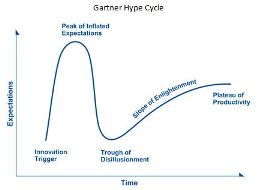
Based on Gartner's June 2017 Hype Cycle for Emerging Technologies, 2017 report, their analysis shows human augmentation devices (industrial exoskeletons) are on the rise moving toward the "peak of inflated expectations" phase. They still need to travel through the "trough of disillusionment" before entering the "slope of enlightenment."
Gartner Hype Cycle
Gartner Methodologies, Gartner Hype Cycle, https://www.gartner.com/technology/research/methodologies/hype-cycle.jsp
Representatives from both industry and academia have similar perspectives.
- Industry: Zach Hass, product manager, Ekso Bionics, recently stated, "That's certainly more than five years away. More than ten, probably, to be able to lift your own body weight with minimal effort. More than 20 until we see real application in a plant." (http://www.cbc.ca/news/technology/ekso-bionics-eksovest-ford-assembly-line-1.4645523)
- Academia: Dr. William Marras, director of The Ohio State University Spine Research Institute and Honda Chair Professor of Integrated Systems Engineering, says, "The simplest way to describe it is like dancing with a really bad partner. Someone is tugging and pulling on you in directions you're not expecting, and your body has to compensate for that. And the way you compensate is by recruiting different muscles to perform the task." (https://news.osu.edu/news/2018/04/20/for-heavy-lifting-use-exoskeletons-with-caution/)
So, hold on a bit longer until the capabilities of these devices match our expectations to improve human performance and reduce MSDs.
References
1. Bosch T, van Eck J, Knitel K, de Looze M. (2016). The effects of a passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Appl Ergon. 2016 May; 54:212-7.
2. de Looze MP, Bosch T, Krause F, Stadler KS, O’Sullivan LW. (2016). Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics. 2016 May;59(5):671-81.
3. Kim S, Nussbaum MA, Mokhlespour Esfahani MI, Alemi MM, Alabdulkarim S, Rashedi E. (2018). Assessing the influence of a passive, upper extremity exoskeletal vest for tasks requiring arm elevation: Part I – "Expected" effects on discomfort, shoulder muscle activity, and work task performance. Appl Ergon. 2018 Mar 7. pii: S0003-6870(18)30059-0. doi: 10.1016/j.apergo.2018.02.025. [Epub ahead of print].
4. Kim S, Nussbaum MA, Mokhlespour Esfahani MI, Alemi MM, Jia B, Rashedi E. (2018). Assessing the influence of a passive, upper extremity exoskeletal vest for tasks requiring arm elevation: Part II – "Unexpected" effects on shoulder motion, balance, and spine loading. Appl Ergon. 2018 Mar 7. pii: S0003-6870(18)30058-9. doi: 10.1016/j.apergo.2018.02.024. [Epub ahead of print]
5. Marras WS. (2012). The complex spine: the multidimensional system of causal pathways for low-back disorders. Hum Factors. 2012 Dec;54(6):881-9.
6. National Research Council & Institute for Medicine. (2001). Musculoskeletal disorders and the workplace: Low back and upper extremity. Washington, DC: National Academy of Sciences, National Research Council, National Academy Press.
7. Rashedi E, Kim S, Nussbaum MA, Agnew MJ. (2014) Ergonomic evaluation of a wearable assistive device for overhead work. Ergonomics. 2014;57(12):1864-74.
8. Theural J, Desbrosses K, Roux T, Savescu A. (2018). Physiological consequences of using an upper limb exoskeleton during manual handling tasks. Appl Ergon. 2018 Feb;67:211-217.
9. Weston EB, Alizadeh M, Knapik GG, Wang X, Marras WS. (2018). Biomechanical evaluation of exoskeleton use on loading of the lumbar spine. Appl Ergon. 2018 Apr;68:101-108.
10. Young AJ, Ferris DP. (2017). State of the Art and Future Directions for Lower Limb Robotic Exoskeletons. IEEE Trans Neural Syst Rehabil Eng. 2017 Feb;25(2):171-182.
This article originally appeared in the October 2018 issue of Occupational Health & Safety.