
Essential Precautions for Health Care, General Industry
CDC's Healthcare Infection Control Practices Advisory Committee divides ATDs into those two categories, diseases requiring Airborne Precautions and diseases requiring Droplet Precautions.
- By Jerry Laws
- May 01, 2016
A Workplace Solutions document1 recently made available by NIOSH on its website gives health care workers and their safety leaders answers to five common myths involving respiratory protection in health care—surgical masks and N95 filtering facepiece respirators. The document includes a simple chart for selecting the right type of respirator based on the task being performed on a patient who has a suspected or confirmed infectious disease.
Included in it is a reference to a much more comprehensive 2015 guidance document, a "Hospital Respiratory Protection Program Toolkit"2 written for respirator program administrators, that offers guidance for understanding hospitals’ respiratory hazards, selecting the appropriate protection, developing a respiratory protection program, developing policies and procedures, and storing and maintaining respirators that are ready for use. Both of these documents specifically address pandemic influenza, with the toolkit explaining that influenza viruses require droplet precautions by workers who could be in contact with patients who may have aerosol transmissible diseases (ATDs). Measles, TB, and some other diseases/pathogens require airborne precautions, it states.
"When Droplet Precautions are recommended, surgical masks function to reduce the transmission of large infectious droplets between the source (patient) and the mucosal surfaces of a susceptible host (healthcare personnel). When Airborne Precautions are recommended, respirators and other control measures, such as patient isolation in an airborne infection isolation room (AIIR) with specialized ventilation, are used to protect healthcare personnel from inhaling infectious particles that are of small diameter, likely to remain infectious over long time or distance, or both," the toolkit explains. It was adapted from a 2012 California guide, "Implementing Respiratory Protection Programs in Hospitals: A Guide for Respirator Program Administrators," which was developed by the California Department of Public Health's Occupational Health Branch and the Public Health Institute under a NIOSH contract.
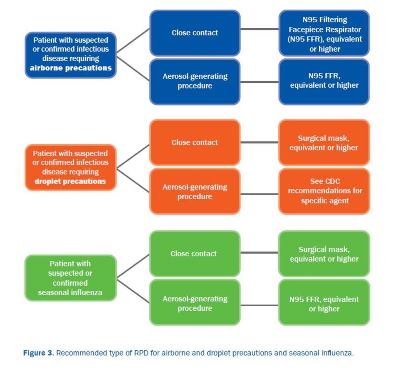
CDC's Healthcare Infection Control Practices Advisory Committee, HICPAC, divides ATDs into those two categories, diseases requiring Airborne Precautions and diseases requiring Droplet Precautions. "The hazards associated with ATDs (e.g., infectious patients with a transmissible disease or, in rare situations, environmental sources of anthrax or fungi) cannot be eliminated from or substituted out of the hospital setting. ATD pathogen exposures cannot routinely be measured in the air, and have no established occupational exposure limits. In addition, ATD pathogens vary in infectivity and severity of outcome. In order to protect employees from ATDs, healthcare facilities must implement comprehensive infection control plans utilizing a combination of engineering, administrative (including training and vaccination), and work practice controls, and provide for the use of respirators and other PPE," it states.
Key Respiratory Program Requirements
The toolkit indicates that a respiratory protection program has nine key requirements:
1. A written program with policies and procedures
2. Program administrator
3. Hazard evaluation and respirator selection
4. Medical evaluation for respirator wearers
5. Fit testing
- Initial
- Annual
- After any physical changes that may affect fit
6. Proper respirator:
- Use
- Storage
- Maintenance
- Repair
- Disposal
7. Training
8. Program evaluation
9. Recordkeeping
General Industry Respiratory Protection
For industrial workers, OSHA's 1910.134 standard specifies respiratory protection requirements, including at (a)(1): "In the control of those occupational diseases caused by breathing air contaminated with harmful dusts, fogs, fumes, mists, gases, smokes, sprays, or vapors, the primary objective shall be to prevent atmospheric contamination. This shall be accomplished as far as feasible by accepted engineering control measures (for example, enclosure or confinement of the operation, general and local ventilation, and substitution of less toxic materials). When effective engineering controls are not feasible, or while they are being instituted, appropriate respirators shall be used pursuant to this section."
Other sections of this standard require the employer to develop and implement a written respiratory protection program that must be administered by a suitably trained program administrator. The required program elements, echoing the toolkit's lineup of key requirements, are listed in 1910.134(c)(1)(i) through 1910.134(c)(1)(viii) and include respirator selection procedures; medical evaluations; fit testing; procedures and schedules for cleaning, disinfecting, storing, inspecting, repairing, discarding, and otherwise maintaining respirators; "procedures to ensure adequate air quality, quantity, and flow of breathing air for atmosphere-supplying respirators"; and employee training both on the respiratory hazards to which they are potentially exposed during routine and emergency situations and in the proper use of respirators.
And even where respirator use is not required, an employer may provide respirators at the request of employees or permit employees to use their own respirators voluntarily, if the employer determines that such respirator use will not in itself create a hazard; if the employer determines that voluntary respirator use is permissible, the employer shall then implement the elements of a written respiratory protection program necessary to ensure that any employee using a respirator voluntarily is medically able to use that respirator and that the respirator is cleaned, stored, and maintained so that its use does not present a health hazard to the user. (Except that employers aren't required to include in a written respiratory protection program the employees whose only use of respirators involves the voluntary use of dust masks.)
References
1. "Preparedness through Daily Practice: The Myths of Respiratory Protection in Healthcare," http://www.cdc.gov/niosh/docs/wp-solutions/2016-109/pdfs/2016-109.pdf
2. https://www.osha.gov/Publications/OSHA3767.pdf
This article originally appeared in the May 2016 issue of Occupational Health & Safety.