Summary:

In 2015, the news about the high lead levels in Flint, Michigan’s drinking water caused the nation to focus its attention on lead. The EPA has a strong regulatory structure for lead in drinking water, yet in 2015, Flint found that lead from its aging pipes was exposing the community to hazardous levels of lead. The circumstances surrounding Flint’s water problem were unique, but other communities across the country are discovering that they too have problems with lead. This has prompted state regulators to lower acceptable drinking water levels and require statewide water testing in schools and day care centers.
History of Lead Use and Exposure

From Rome to Flint
Lead is a naturally occurring, inert metal that was one of the earliest metals used by the human race. There is ancient evidence of lead use by humans as early as 3000 B.C. It was the metal used in ancient Roman piping to distribute water from its celebrated aqueduct system. The word plumber comes from the Latin word plumbum, meaning lead.
In the modern age, lead has been widely used in paints, pipes, solder, gasoline, batteries, glass, and pottery. And even with regulations limiting its use, lead-based or lead-containing products are still found in construction, military, and marine applications, and even recently in toys, jewelry, furniture, imported food, and other products.
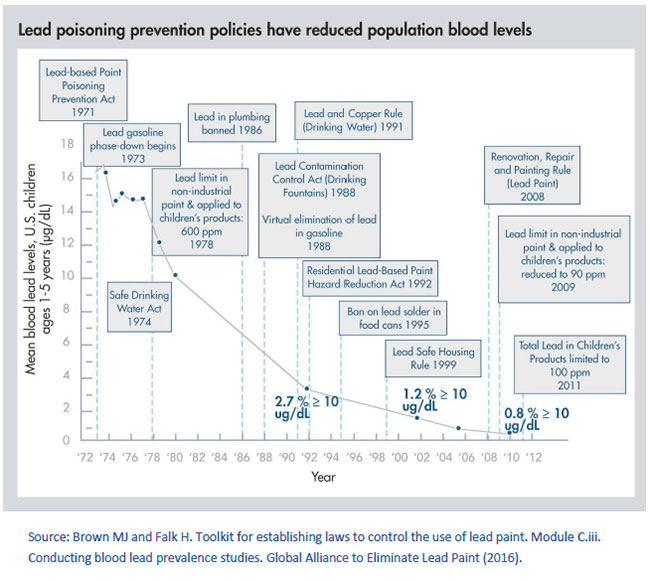
Lead exposure litigation was front-page news throughout the 1970s and into the 1990s, with class action suits brought in Baltimore, New York, and other large cities, as a result of child lead poisonings from the paint in residential complexes. This prompted a myriad of actions by various governmental agencies, including the Center for Disease Control (CDC); Environmental Protection Agency (EPA); Department of Housing and Urban Development (HUD); National Institute for Occupational Safety and Health (NIOSH); and the Occupational Safety and Health Administration (OSHA). They conducted public health population studies, lowered the acceptable blood-level limits in children and adults, and enacted local and Federal regulations to ban uses of lead and clean up environmental hazards created by its use. These regulations resulted in a significant reduction of lead exposure hazards associated with gasoline, paints, and solder. But despite significant reductions, lead hazards were not eliminated. The figure below illustrates the impact of these regulations on the mean childhood blood lead levels between 1971 and 2012.1
Flint and Beyond
In 2015 the lead contaminated water in Flint, Michigan made front page news. Flint’s water problems stem from an ill-fated attempt to save money by disconnecting from the Detroit Water and Sewerage Department, which had provided the city with safe water from Lake Huron for decades and start using the water from the Flint River. In subsequent State legislative hearings on the crisis, it emerged that the Flint River water needed inexpensive chemicals that would have helped prevent the pipe corrosion that caused the lead to leach into the water. But before the anti-corrosion chemicals could be added, the City needed to upgrade its equipment, which would have cost millions of dollars. About half of the piping to the homes in Flint contained lead that began leaching into the water being used by thousands of residents. Virginia Tech researchers identified the problem and sounded the alarm. A local public health crisis erupted, which prompted concern by other cities’ health authorities.

Despite New York City proudly proclaiming that its highly-protected water supply from Upstate New York water supply is clean, the City found lead in school water. New York is not alone; lead contamination in school water is being reported all over the country. There have also been recent media reports of elevated lead levels in school water in Richmond, VA; Phoenix, AZ; New Brunswick, NJ; Mountain View, CA; and Berkeley, CA. As much of the nation’s water distribution system is aging, there will likely be more troubling news.
Sources of Contamination and Health Effects
Ingestion and Inhalation
Lead poisoning can occur in children and adults. In children, poisoning typically occurs by ingesting (swallowing) soil contaminated by lead, lead-containing paint, foods and water, cookware, and toys. In adults, the pathway is mostly occupational (inhalation or ingestion). In the United States, 14–20% of total lead exposure is attributed to drinking water.
Blood Lead Levels
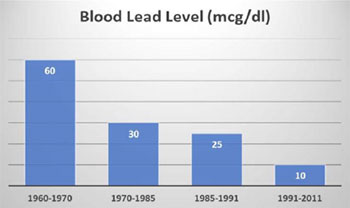
The CDC has defined the blood-lead level (BLL) to determine whether an individual has been poisoned. As new information has emerged about the toxic effects of lead exposure and as more sensitive detection methods are developed, the CDC has progressively lowered the BLLs for lead exposure (see the figure below illustrating BLLs between 1960-2011).2
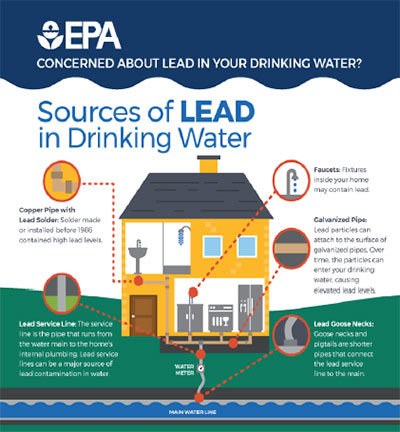
In 2012, the CDC adopted an advisory level for environmental and educational intervention of five micrograms per deciliter (5 μg/dL) as the upper reference range value for BLLs in children.3 Today, the CDC estimates that there are 4 million households in the US with children living with high lead levels and that there are still 24 million homes with lead-based paint contamination. The CDC defines no safe blood lead level and has recognized that exposure risks can often be influenced by social and economic factors. In 2016, the EPA updated its programs to require lead-based paint training for individuals involved in certain building trades, as well as certain types of contractors, real estate professionals, day care centers, schools, and contractors involved in removing lead materials. According to the Poisoning Prevention Program, it is the combined goal of HUD, EPA, and the CDC to eliminate childhood lead poisoning as a public health problem by the year 2020. The number of homes, buildings, and schools serviced by lead-containing water piping is unknown. However, the water distribution systems in urban settings and in homes constructed prior to 1970 may contain lead-containing components. The EPA diagram below illustrates multiple potential sources of lead in home drinking water distribution systems.4
Lead Poisoning in Children and Adults
 Lead is a neurotoxin, meaning that it effects the nervous system. The symptoms that children experience, depending on exposure levels and the duration of exposure, may include death, coma, seizures, encephalopathy, brain damage, and kidney dysfunction. However, the more common effects on children include decreased IQ scores, attention and behavioral problems, speech and language disorders, learning disabilities, and problems with motor and sensory skills. Poisoning usually occurs between the ages of 1 to 6, but the effects can be long lasting.
Lead is a neurotoxin, meaning that it effects the nervous system. The symptoms that children experience, depending on exposure levels and the duration of exposure, may include death, coma, seizures, encephalopathy, brain damage, and kidney dysfunction. However, the more common effects on children include decreased IQ scores, attention and behavioral problems, speech and language disorders, learning disabilities, and problems with motor and sensory skills. Poisoning usually occurs between the ages of 1 to 6, but the effects can be long lasting.
Adults symptoms of lead poisoning may include abdominal pain, fatigue, headaches, irritability, memory loss, weakness, depression, distraction, and high blood pressure. There is also a risk of fetal exposure and infertility. Common at-risk occupations include construction trades in older buildings, artists, auto mechanics, bridge reconstruction, glass manufacturing, miners, smelting, electrical workers, and plumbers/pipe fitters.
Do I Have a Problem: Testing
Several states have recently implemented extensive testing requirements in schools and day care centers. The California Department of Education has recently required that all public K-12 schools built before 2010 must test their water for lead by mid-2019. This was after lead issues were discovered in San Diego and Sacramento public schools. Michigan has recently proposed requiring communities to test annually and has lowered its action level for lead in drinking water to a level that is below the current federal action level. Illinois has recently required lead testing in all commercial and residential day care centers.
Testing drinking water systems to determine its lead concentration is relatively easy and inexpensive. Because of the increased media attention on the lead problem, many health agencies are overwhelmed and cannot sample every potential water source. Often, the quickest way to determine if your water is free of lead contamination is to contact a local industrial hygiene or environmental services company. They typically have the required knowledge and experience required to collect a sample of your water, have it analyzed by an accredited lab, and tell you whether you have a problem.
About RHP Risk Management
RHP Risk Management is a leader in the field of Industrial Hygiene and Occupational Safety. We specialize in the evaluation of exposure to chemicals, noise, vapors, hazardous materials, and biological contaminants, in your workplace and in our state-of-the-art Exposure Simulation Laboratory.
1https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf, CDC, Key Federal Programs to Reduce Childhood Lead Exposures and Eliminate Associated Health Impacts, President’s Task Force on Environmental Health Risks and Safety Risks to Children, November 2016, Accessed 3-28-2018
2 https://www.atsdr.cdc.gov/csem/csem.asp?csem=7&po=8#tocbookmark2, ATSDR- CDC, Lead Toxicity
What Are the U.S. Standards for Lead Levels?, Accessed 12-16-2016
3 https://www.atsdr.cdc.gov/csem/csem.asp?csem=7&po=8#tocbookmark2, ATSDR- CDC, Lead Toxicity
What Are the U.S. Standards for Lead Levels?, Accessed 12-16-2016
4 https://www.epa.gov/sites/production/files/2017-08/documents/epa_lead_in_drinking_water_final_8.21.17.pdf, US EPA Sources of Lead In Drinking Water – 2017, Accessed 3-28-2018